Delaware Insurance Commissioner Karen Weldin Stewart announced that insurers will issue more than $2 million in rebates to 14,399 health insurance policyholders in Delaware as a result of the Affordable Care Act’s 80/20 medical loss ratio rule.
The rule requires insurers in the individual and small group markets to spend at least 80 percent of premium dollars on medical costs and activities that improve the quality of health care, and no more than 20 percent on administrative costs, including executive salaries, overhead and marketing.
In the large group market, the ratio is higher — insurers must spend at least 85 percent of premiums on health care and quality improvements.
Any company selling health insurance in Delaware that fails to meet these standards will owe policyholders a refund. Rebates for individual market premiums are paid directly to the consumers, while those for small and large groups are paid to the employer who purchased those group plans.
Rebates may take the form of a check in the mail, a lump-sum reimbursement to a bank account (if the premium was paid by credit or debit card), or a direct reduction in future premiums.
The following chart provides a list of those insurers who owed rebates to Delaware consumers based on their medical loss ratio for coverage year 2014. Any company not listed equaled or exceeded the medical loss ratio requirement:
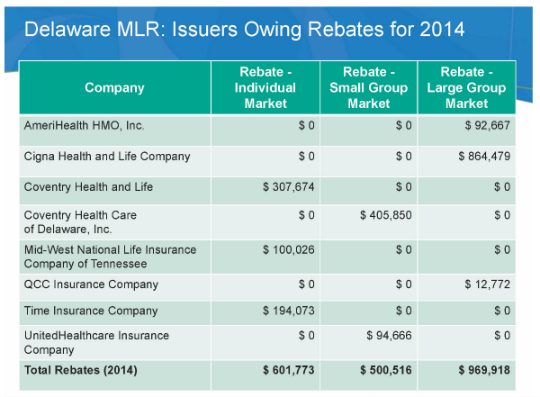
Source: The Delaware Department of Insurance
Was this article valuable?
Here are more articles you may enjoy.


 Florida Engineers: Winds Under 110 mph Simply Do Not Damage Concrete Tiles
Florida Engineers: Winds Under 110 mph Simply Do Not Damage Concrete Tiles  Insurance Broker Stocks Sink as AI App Sparks Disruption Fears
Insurance Broker Stocks Sink as AI App Sparks Disruption Fears  Florida Insurance Costs 14.5% Lower Than Without Reforms, Report Finds
Florida Insurance Costs 14.5% Lower Than Without Reforms, Report Finds  Insurify Starts App With ChatGPT to Allow Consumers to Shop for Insurance
Insurify Starts App With ChatGPT to Allow Consumers to Shop for Insurance 

